FAQs on Medicare Coverage of Telehealth - Kaiser Family Foundation
Telehealth, the provision of health care services to patients from providers who are not at the same location, has experienced a rapid escalation in use during the COVID-19 pandemic, among both privately-insured patients and Medicare beneficiaries. Prior to the pandemic, telehealth utilization among traditional Medicare beneficiaries was extremely low, with only 0.3% of traditional Medicare beneficiaries enrolled in Part B using telehealth services in 2016. Between 2019 and 2020, the number of telehealth visits in traditional Medicare increased 63-fold. During the first year of the pandemic, more than 28 million Medicare beneficiaries overall used telehealth services, including almost half (49%) of Medicare Advantage enrollees and nearly 4 in 10 (38%) beneficiaries in traditional Medicare.
These FAQs provide answers to questions about Medicare's current coverage of telehealth, changes made at the outset of the public health emergency, additional changes adopted by Congress and the Administration, and some of the policy considerations that lie ahead.
What is the current scope of Medicare telehealth coverage and how did it change at the start of the COVID-19 pandemic?
Under current law and regulations, Medicare covers a broad scope of services via telehealth without restrictions that were in place prior to the COVID-19 pandemic, but, for the most part, this broader coverage is available only temporarily. People with Medicare can now access telehealth services, whether in urban or rural areas, at home or in other settings, using audio-visual or audio-only technologies, and from a wide range of health care providers. This is due to a broad but time-limited expansion of telehealth coverage in Medicare during the COVID public health emergency. To make it easier and safer for beneficiaries to seek medical care during the pandemic, in March 2020, the Secretary of the Department of health and Human Services (HHS) waived certain restrictions on Medicare coverage of telehealth services for Medicare beneficiaries during the COVID-19 public health emergency, based on waiver authority included in the Coronavirus Preparedness and Response Supplemental Appropriations Act (and as amended by the CARES Act) (Figure 1). The public health emergency was most recently renewed in April 2022, and the Biden Administration has said that it will provide a 60-day notice before allowing the public health emergency to expire. Because the Biden Administration has not yet provided a 60-day notice that the public health emergency will end, it is likely the PHE will extend beyond July.
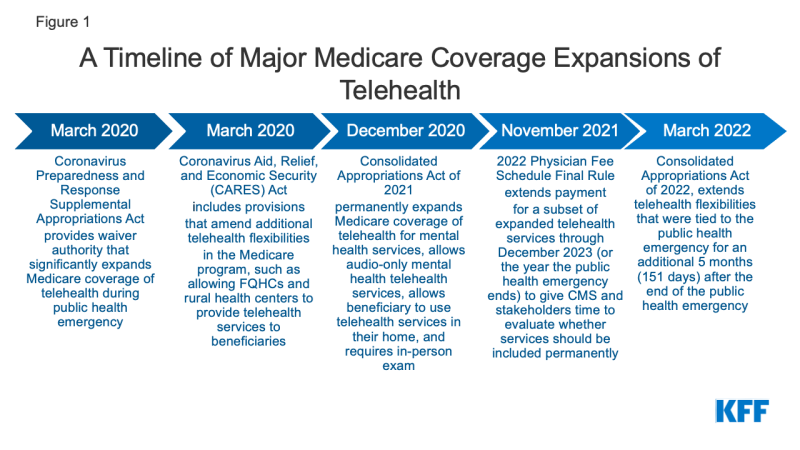
Figure 1: A Timeline of Major Medicare Coverage Expansions of Telehealth
The Consolidated Appropriations Act of 2022 (CAA of 2022) extended many of the recent expansions of Medicare's telehealth coverage for roughly 5 months (151 days) after the end of the COVID-19 public health emergency. This means, for example, if the public health emergency ends in October 2022, Medicare coverage of telehealth would revert to more limited coverage in March 2023, and most beneficiaries in traditional Medicare would lose access to telehealth coverage for most services, except for mental health services (see below for more information). This is because before the pandemic, coverage of telehealth services under Medicare was limited to rural beneficiaries using telehealth at an "originating site," such as a clinic or doctor's office, rather than from their own homes. There were also restrictions on which providers could be paid to deliver telehealth services (i.e., "distant site" providers). There was also a relatively limited set of services that could be covered by telehealth. (Medicare Advantage plans have flexibility to offer additional telehealth benefits beyond those that are covered by traditional Medicare outside of the public health emergency, as described below).
What services can Medicare beneficiaries receive through telehealth?
Before the public health emergency, Medicare covered about 100 services that could be administered through telehealth, including office visits, psychotherapy, and preventive health screenings, among other services. During the public health emergency, the list of allowable telehealth services covered under Medicare has expanded to include emergency department visits, physical and occupational therapy, and certain other services. Some evaluation and management, behavioral health, and patient education services can be provided to patients via audio-only telephone.
In the 2022 physician fee schedule final rule, the Centers for Medicare & Medicaid Services (CMS) temporarily extended coverage for a subset of the expanded telehealth services through December 31, 2023 (or through the end of the year in which the public health emergency ends, whichever is later) to give both CMS and stakeholders time to evaluate whether they should be permanently included as Medicare-covered telehealth services. These services include physical and occupational therapy, end-stage renal disease (ESRD) visits, emergency department visits, critical care services, and others.
What mental health telehealth services are available for Medicare beneficiaries?
Telehealth has played an important role during the COVID-19 pandemic in providing access to mental health services for older adults, one in four of whom reported anxiety or depression in August 2020. During the first year of the pandemic, a large share of Medicare beneficiaries' behavioral health services were conducted via telehealth, and a larger share of behavioral health services were delivered via telehealth for beneficiaries in traditional Medicare (16%) than enrollees in Medicare Advantage (9%).
Based on provisions in the Consolidated Appropriations Act of 2021, policymakers have permanently expanded coverage for telehealth services for the purpose of diagnosis, evaluation, or treatment of mental health disorders after the end of the COVID-19 public health emergency. Medicare beneficiaries can use telehealth for mental health services in their homes, and beneficiaries who cannot use real-time two-way audio and video for telehealth mental health services are permitted to use audio-only devices to access these services. Beneficiaries are required to have an in-person, non-telehealth service within six months of their first telehealth mental health service (although the CAA of 2022 delayed this requirement for 151 days after the end of the public health emergency).
What do Medicare beneficiaries pay for telehealth services?
Beneficiary cost sharing for telehealth services has not changed during the public health emergency. Medicare covers telehealth services under Part B, so beneficiaries in traditional Medicare who use these benefits are subject to the Part B deductible of $233 in 2022 and 20% coinsurance. However, the HHS Office of Inspector General has provided flexibility for providers to reduce or waive cost sharing for telehealth visits during the COVID-19 public health emergency, although there are no publicly-available data to indicate the extent to which providers may have done so. Most beneficiaries in traditional Medicare have supplemental insurance that may pay some or all of the cost sharing for covered telehealth services. Medicare Advantage plans have flexibility to modify cost-sharing requirements provided they meet standards of actuarial equivalence and other CMS requirements.
What technologies can be used for telehealth services?
During the COVID-19 public health emergency, telehealth services covered by Medicare can be conducted via an interactive audio-video system, as well as using smartphones with real-time audio/video interactive capabilities without other equipment. Additionally, a limited number of telehealth services can be provided to patients via audio-only telephone or a smartphone without video (such as telephone evaluation and management services and behavioral health counseling).
When the 151-day period after the public health emergency ends, a telehealth visit must be conducted with two-way audio/video communications; the use of audio-only telephones will not be permitted, except for mental health services (as described above).
What type of providers can get reimbursed by Medicare for telehealth services?
During the public health emergency, any health care professional who is eligible to bill Medicare for professional services can provide and bill for telehealth services and does not need to have previously treated the beneficiary. Also, federally qualified health centers and rural health clinics are eligible for reimbursement for telehealth services provided to Medicare beneficiaries during the COVID-19 public health emergency; these settings were not authorized as providers of telehealth services for Medicare beneficiaries prior to statutory and regulatory changes made at the beginning of the pandemic.
If no other statutory changes are made, once the 151-day period after the public health emergency ends, Medicare reimbursement for telehealth will revert to rules in place before the public health emergency. Under these rules, only physicians and certain other practitioners (such as physician assistants, clinical social workers, and clinical psychologists) will be eligible to receive Medicare payment for telehealth services provided to eligible beneficiaries in traditional Medicare, and they must have treated the beneficiary receiving the services in the last three years.
How does Medicare pay providers for telehealth services?
During the public health emergency, Medicare pays for telehealth services, including those delivered via audio-only telephone, as if they were administered in person, with the payment rate varying based on the location of the provider, which means that Medicare pays more for a telehealth service provided by a doctor in a non-facility setting, such as a clinician's office, than by a doctor in a facility setting, such as a hospital outpatient department. This also means that during the public health emergency, doctors in non-facility settings are receiving a higher payment for services provided by telehealth than they did before the public health emergency.
Assuming no changes to current law, Medicare's payment for a telehealth service after the 151-day period after the public health emergency ends will be the same regardless of whether it was provided in a non-facility setting or a facility setting, and the payment rate will be based on the lower amount paid to facility-based providers for a service delivered in person. (Under Medicare's physician fee schedule, the payment to facility-based-providers for in-person services is lower than the payment to non-facility providers because Medicare makes a separate payment to facilities to cover practice expenses, such as physical space, medical supplies, medical equipment, and clinical staff time.) The rationale for using the lower facility payment amount for telehealth services is that practice expenses for the delivery of telehealth services should be lower than those for an in-person visit.
How do Medicare Advantage plans cover telehealth?
Medicare Advantage plans are required to cover all Part A and Part B benefits covered under traditional Medicare. Additionally, since 2020, Medicare Advantage plans have been able to offer telehealth benefits not routinely covered by traditional Medicare (that is, not during the COVID-19 public health emergency), including telehealth services provided to enrollees in their own homes and services provided outside of rural areas. In 2022, virtually all Medicare Advantage plans (98%) offer a telehealth benefit. During the first year of the COVID-19 pandemic, 49% of Medicare Advantage enrollees used telehealth services.
Medicare Advantage plans are paid a capitated amount by Medicare to provide basic Medicare benefits covered under Parts A and B, including telehealth services. Plans are now permitted to include costs associated with additional telehealth benefits (beyond what traditional Medicare covers) in their bids for basic benefits.
Medicare Advantage plans have flexibility to waive certain requirements with regard to coverage and cost sharing in cases of disaster or emergency, such as the COVID-19 pandemic. CMS has advised plans that they may waive or reduce cost sharing for telehealth services, as long as plans do this uniformly for all similarly-situated enrollees. Many Medicare Advantage plans have waived or reduced cost sharing for enrollees for some or all services administered via telehealth during the public health emergency.
How is telehealth covered under Medicare for beneficiaries and providers participating in alternative payment models?
Like all other traditional Medicare beneficiaries, beneficiaries who receive care through an alternative payment model can access expanded telehealth benefits during the public health emergency. Separate from the time-limited expanded availability of telehealth services, CMS has granted providers participating in some alternative payments models, including Medicare Shared Savings Program ACOs, greater flexibility to provide care through telehealth, including billing for telehealth services provided to both urban and rural beneficiaries and to beneficiaries when they are at home.
Will Medicare's coverage of "virtual check ins" expire at the end of the public health emergency?
Separate from Medicare's coverage of telehealth services, Medicare covers brief, "virtual check-ins" (also called "brief communication technology-based services") via telephone or captured video image, and E-visits for all beneficiaries, regardless of whether they live in a rural area. Both virtual check-ins and E-visits, which were available to all beneficiaries prior to the public health emergency and will continue to be available to all beneficiaries after the public health emergency, are more limited in scope than a full telehealth visit. For example, virtual check-ins can only be reported by providers with an established relationship to the patient, cannot be related to a recent medical visit (within the past 7 days), and cannot lead to a medical visit in the next 24 hours (or the soonest available appointment), and payment is intended to cover only 5-10 minutes of medical discussion.
What are current legislative proposals to expand Medicare coverage of telehealth?
Policymakers are considering a variety of proposals to expand some or all of the existing flexibilities surrounding telehealth services under Medicare beyond the public health emergency, and many have expressed support for doing so. Among the telehealth-related bills that have been introduced in the 117th Congress are proposals to extend certain Medicare telehealth services and to permanently lift geographic and site-based restrictions for Medicare coverage of telehealth. Other legislation would permanently cover some of the telehealth expansions provided during the public health emergency and expand the scope of providers eligible for payment for telehealth services covered by Medicare. Other bills are aimed at assessing the impact of expanded telehealth services in Medicare and Medicaid on utilization of telehealth visits, including by demographics.
What policy issues are under consideration regarding the future of telehealth coverage under Medicare?
Expanded coverage of telehealth beyond the COVID-19 public health emergency could affect the quality of patient care as well as program and beneficiary spending. Broadening telehealth coverage has the potential to improve access to needed care, but the implications of telehealth for communities of color are not yet clear, with research showing both higher use in disadvantaged neighborhoods and lower use among black and rural Medicare beneficiaries than white beneficiaries. Moreover, expanding telehealth coverage would likely lead to an overall increase in Medicare program spending: CBO scored five months of expanded telehealth coverage included in the CAA 2022 as costing $663 million. However, some telehealth services may be substitutes for in-person care, such as a behavioral health care visit, though easier access to telehealth could lead to an overall increase in visits and costs. Other telehealth services may not fully replace the need for (or occurrence of) an in-person visit, such as when lab work is determined to be needed.
Additionally, state licensing requirements could affect access to telehealth services. During the public health emergency, states used emergency authority to waive aspects of state licensing requirements for medical providers to make it easier for people to access health care via telehealth, and many of these waivers are ending. More than half of states have signed the Interstate Medical Licensure Compact, which creates an expedited pathway for state licensure for medical providers, although it does not provide reciprocity for providers who have a state license in one state and want to practice in another.
The potential expansion of telehealth coverage brings with it concerns about the potential for fraudulent activity. There have been several large fraud cases involving telehealth companies in recent years, most of which involved the submission of fraudulent claims for items, services, and tests to Medicare and other insurers that were never given or administered to patients. HHS' Office of the Inspector General (OIG) is conducting several studies to assess the appropriateness of use of telehealth during the public health emergency, including an analysis of provider billing patterns in order to identify providers that could pose a risk for program integrity and an audit of telehealth services under Part B to assure that services are meeting Medicare requirements. The Medicare Payment Advisory Commission (MedPAC) has recommended that Medicare apply additional scrutiny to outlier clinicians who deliver more telehealth services than others, as well as requiring in-person visits before clinicians can order high-cost equipment or services for beneficiaries.



Comments
Post a Comment