Decreasing reproductive and abortion care barriers: findings on the ... - BioMed Central
We invited students to respond to an anonymous online survey to understand students' self-reported use of and attitudes toward reproductive and abortion services. We conducted this survey in anticipation of legislated medication abortion provision at California public university campuses starting in 2023.
Recruitment
The study population was students at a minority-serving institution (MSI) public university in a large coastal Northern California city consisting of a diverse, majority-commuter student population, where 60.13% of undergraduate students receive federal aid and 42.58% receive Pell Grant funding [16]. Recruitment for the anonymous web-based quantitative survey was done via on-campus and virtual methods to reflect hybrid learning modalities at the university due to the COVID-19 pandemic. Eligible respondents were self-reported students aged 18 and over. We posted and distributed recruitment flyers with QR codes on campus at residence halls, academic buildings, the library, wellness (athletic) center, SHC, food court, and Student Union. We used college listserver emails inviting students to participate in a "Reproductive Health and Access Study" via a live link. We posted the survey announcement in the online student life hub calendar. Survey data was collected on the Qualtrics platform from March 01, 2022–May 02, 2022.
Measures
The distributed survey contained 9 modules, with response-based skip patterns determining the survey length for each participant. Most participants spent between six to eleven minutes responding to the survey. Measures included demographic characteristics (gender identity, age, race/ethnicity, learning modality, anticipated degree, employment status, insurance status, housing situation, distance from campus); and validated instruments that ask about use, access and attitudes toward reproductive and sexual health products and services including pregnancy tests, emergency contraception pills, and medication abortion. The survey participants reported previous and preferred locations for use of products and services at five types of healthcare settings; knowledge of whether they could access this healthcare in their community; and sexual and reproductive healthcare behaviors including preventing STIs and pregnancy as applicable. Our assessment of student self-reported use and location knowledge of sexual and reproductive health products and services included barriers to this healthcare overall, and in the context of accessing on-campus student health services, across demographic characteristics.
Barriers to care
The study sought to understand the types and extent of barriers students face in accessing reproductive care. We asked participants to report which barriers make it difficult for them or their partner(s) to access reproductive health products and services generally. They were then asked which issues (barriers) have made, or would make, it difficult to access care at the SHC at their university. Both questions provided a multi-option list; respondents could check off as many answers as they wanted. An "Other: Please specify" response option was available.
To analyze types of barriers experienced generally and at the SHC across the sample population and by demographic subgroups, we categorized question response options into three constructs: (a) Stigma, (b) Access, and (c) System Barriers. Figure 1 details the response options included in each construct.
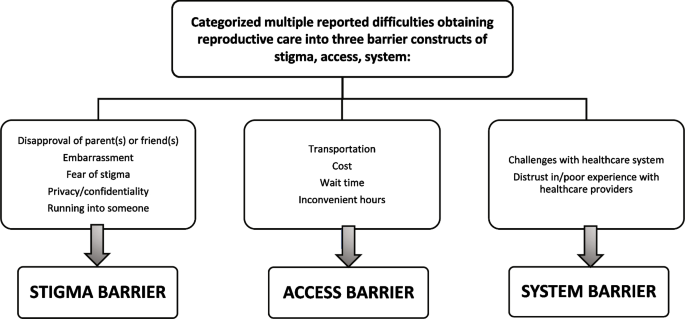
Categorization of barriers to obtaining reproductive & on campus healthcare
Knowledge of reproductive & sexual healthcare availability
We asked respondents if they knew at least one location in their community where a series of reproductive and sexual health products and services are available. We focused on three services: (1) pregnancy test, (2) emergency contraception pills, and (3) medication abortion. These were selected to reflect an increasingly complex stepwise progression of care for those respondents with the potential for themselves or their partner(s) to become pregnant. A pregnancy test is a product than anyone can purchase without appointment or consultation. Emergency contraception pills are available for over-the-counter (OTC) purchase but require a limited appointment for those needing advice, informational instructions to receive the most effective option for those who weigh over 195 pounds, or payment support through insurance or subsidy program. Lastly, the current U.S. Food and Drug Administration (FDA) and legislation-mandated care model for medication abortion provision requires the highest level of scheduling, clinical supervision and intervention from the healthcare system [17].
Attitudes toward use of SHC for reproductive healthcare
We asked respondents if as a student they access the SHC at their university and if they would go to the SHC if they or their partner(s) needed a series of reproductive health products and services. We asked respondents if they would recommend using the SHC to a friend who needed these products and/or services. We focused our analysis on pregnancy test, emergency contraception pills (ex: "morning after pill," "Plan B," or "Ella"), and medication abortion.
Demographic group measures
To better understand the extent to which certain barriers were most relevant to specific populations and for which populations further outreach and support may be required to address inequities, we categorized responses to be as inclusive as possible. For gender identity, we created a three-category variable of female, male, and transgender/gender expansive (trans/GE). Respondents were categorized as trans/GE who selected: Transgender (n = 2); Nonbinary (n = 9); and Other—Please specify ("Genderqueer" [n = 1]; "He/They" [n = 1]). For race and ethnicity, we allowed respondents to choose from several standard groups (African American, Asian, Pacific Islander, Latino/a, white, mixed race) and also to self-identify into an "other" category. We examined race/ethnicity individually where we had sufficient data, but there were too few Pacific Islanders and "other" respondents to analyze these groups independently. To include respondents across all demographic groups in the analysis, we also further collapsed self-reported racialized and ethnic identities into a three-category variable including (a) underrepresented minority students (URM; African American, Latinx and Pacific Islander), (b) non-underrepresented minority students (non-URM; White and Asian American) and (c) Mixed race/ethnicity students.
Statistical analyses
We report survey means and 95% confidence intervals to compare barrier types by setting, general (community) reproductive healthcare versus SHC. We examine chi-square tests to analyze differences in barriers by demographic groups. To compare knowledge of where to get services and whether respondents would use or recommend the SHC for each service, we present mean and 95% confidence intervals for each service. We used STATA17 statistical software for all analyses [18].
Institutional review board approval statement
The University Institutional Review Board provided ethics approval for this study (Protocol 2020-106).



Comments
Post a Comment