Acquired Hemophilia A Post-COVID-19 Vaccination: A Case Report ...
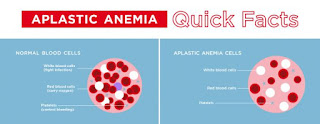
Aplastic Anemia: A Rare Disorder With Severely Low Blood Cell Count
The symptoms of aplastic anemia are mainly related to the low blood cell counts . Aplastic Anemia is believed to be more common in India. Here's all you need to know about this rare disorder.Aplastic anemia is a rare and serious medical condition characterized by a significant decrease in the number of blood cells in the body. The term "aplastic" refers to the failure of the bone marrow to produce enough blood cells, including red blood cells, white blood cells, and platelets. It is an uncommon condition, affecting about 6 per million of population. However, it is believed to be more common in India.
We spoke to Dr. Sweta Lunkad, Consultant Haematologist and BMT specialist, Jupiter Hospital, Pune, to know more about this condition. Excerpts follow:
Causes of Aplastic AnemiaAplastic anemia can be acquired or inherited, and the causes may vary:
Acquired Aplastic Anemia: This form is more common and can be triggered by several factors, including:
Inherited Aplastic Anemia: This form is much rarer and is usually caused by genetic mutations passed down from parents to children.
Symptoms ofAplastic AnemiaThe symptoms of aplastic anemia are mainly related to the low blood cell counts and can vary in severity. Common symptoms include:
Aplastic anemia is diagnosed through a series of tests, which may include:
The treatment for aplastic anemia depends on the severity and underlying cause of the condition.
Options may include:
It's crucial to work closely with a hematologist or a specialist in blood disorders to determine the most appropriate treatment plan for each individual case of aplastic anemia. Early diagnosis and treatment are most imperative in improving the prognosis and quality of life for those affected by this rare condition.
Total Wellness is now just a click away.Follow us on
Don't Miss Out on the Latest Updates.Subscribe to Our Newsletter Today!
Subscribe Now
What To Know About A Low Platelet Count And Chemotherapy
A low platelet count is a common side effect of chemotherapy. If your platelet counts drops too low, your doctor may reduce, delay, or discontinue chemotherapy treatment.
Platelets are special blood cells that help your blood clot. A low platelet count is medically known as thrombocytopenia.
If you have thrombocytopenia, you may have symptoms such as:
You can develop thrombocytopenia for many reasons, including undergoing chemotherapy. When chemotherapy is the underlying cause, it's called chemotherapy-induced thrombocytopenia.
A normal platelet count is usually considered between 150 and 450 billion platelets per liter of blood. Chemotherapy-induced thrombocytopenia is usually defined as a platelet count under 100 billion per liter.
This article will look at how chemotherapy affects your platelet count and how chemotherapy-induced thrombocytopenia is treated.
Chemotherapy (also referred to as chemo) drugs contain chemicals that destroy cancer cells or slow down their growth. These chemicals act broadly on all cells in your body that replicate quickly. The cells in your bone marrow that create platelets are particularly prone to damage from chemo.
A reduced platelet count is a common chemotherapy side effect. In a recent study, researchers found that 13% of more than 15,000 people with solid tumors developed thrombocytopenia within 3 months of starting chemo treatment.
Chemotherapy-induced thrombocytopenia is divided into grades based on its severity:
Chemotherapy regimens and platelet countMany types of chemo drugs are used to treat cancer, and doctors often administer multiple drugs at the same time to target cancer cells in different ways.
Some drugs or combinations of drugs come with a higher risk of damaging your platelets than others.
In a 2020 study, researchers examined the rates of thrombocytopenia among 523 people undergoing treatment for a type of non-Hodgkin's lymphoma called diffuse large B-cell lymphoma.
They reported the following rates:
If you develop thrombocytopenia, future doses of chemotherapy may be:
There's no universally agreed-on minimum platelet count for when doctors decide to delay or discontinue chemotherapy. Your doctor will use their best judgment based on your symptoms and the results of your blood tests to decide when you may be able to resume treatment.
Your doctor may want to administer chemo and radiation therapy with caution at platelet levels under 100 billion per liter. A platelet count of less than 50 billion per liter of blood can complicate surgery.
You usually wouldn't have bleeding complications or need platelet transfusion unless your platelet count drops under 25 billion per liter.
You may need a platelet transfusion if your platelet count drops severely low or if you have bleeding complications.
A platelet transfusion involves injecting platelets from donors into your blood. Unlike red blood cells, platelets don't have blood types so you can receive platelets from almost anybody. Often platelets in transfusions come from 6–10 units of donated platelets.
When do doctors recommend platelet transfusions?Doctors usually only recommend platelet transfusions if your platelet count drops severely low or if you're having reoccurring bleeding complications.
Some chemo regimens are more likely to drop your platelet low enough for you to require a platelet transfusion than others. Here are some examples of low platelet rates based on different cancer regimens:
Medications for low platelet countNo drugs have been FDA-approved to specifically treat chemotherapy-induced thrombocytopenia.
Drugs called antifibrinolytic agents are currently being tested for treatment of thrombocytopenia, but the results and benefits aren't yet known. These drugs help your blood clot by breaking down a protein called fibrin.
Supporting treatmentTreating other causes of thrombocytopenia may help raise your platelet count. Treatment might consist of:
Taking steps to avoid bleeding or bruising may help reduce thrombocytopenia complications. Steps you can take include:
Chemicals in chemotherapy drugs can damage healthy cells in your body that replicate quickly. The cells in your bone marrow that produce platelets are particularly vulnerable to damage from chemo.
A low platelet count is a common side effect of chemo. Platelet counts often return to normal within 4–6 days. If your platelet count drops too low, your doctor may reduce, delay, or discontinue chemo treatment.
Having Myelodysplastic Syndrome (MDS)-associated Anemia: What To Know
Myelodysplastic syndromes (MDS) are a group of blood cancers that affect the bone marrow and can result in a low levels of blood cells. When MDS affects red blood cells, it can lead to anemia in some people.
A low red blood cell count (hemoglobin) is a key feature of anemia. With MDS, anemia occurs because the bone marrow does not work correctly. This can be due to several reasons, including the accumulation of irregular cells in the bone marrow and the bone marrow not producing blood cells properly.
MDS-associated anemia can lead to symptoms such as fatigue, weakness, and pale skin. Treatment usually involves addressing the underlying cause of MDS. Many supportive measures are available to help improve a person's quality of life.
Read on to learn more about anemia with MDS, including symptoms, causes, and treatment. This article also discusses the outlook for MDS.
Anemia is relatively common in people with MDS:
What causes MDS?While the exact cause of MDS is unclear, experts speculate that changes in the DNA of the bone marrow's stem cells contribute to the disease. Other factors that could play a role in the development of MDS include aging because aging stem cells are more likely to develop abnormalities.
MDS can cause low levels of different types of blood cells in the bone marrow.
Also, the following may increase a person's risk of developing MDS:
Anemia associated with MDSIn MDS, anemia develops because the bone marrow is not working properly.
Irregular or immature cells may accumulate in the bone marrow, crowding "normal" red blood cells. Or, the MDS may mean that the bone marrow cannot make red blood cells properly.
Anemia in MDS can lead to the following symptoms:
These are typical symptoms of anemia, even if MDS is not the underlying cause.
However, a person's symptoms can depend on other factors, including the underlying cause of anemia. If MDS is the underlying cause, symptoms may differ according to how far advanced the MDS is.
Learn more about the symptoms of MDS here.
To diagnose MDS-associated anemia, doctors will do the following:
The tests will usually involve a complete blood count to check the blood levels of:
Lab technicians can also assess the size, shape, and number of blood cells using a blood smear.
Doctors might also decide to check for atypical levels of other substances, such as:
Doctors may also recommend bone marrow testing. These tests can identify any irregularities relating to the number, type, size, and shape of blood cells and any changes to the cell's genes.
Treatment options for anemia and MDS are detailed below:
Treating anemiaDoctors treat anemia by finding and treating the underlying cause. This could involve avoiding exposure to a particular chemical or MDS medication.
Treatment aims to improve red blood cell counts. This can bring symptom relief and improve a person's quality of life.
A person may receive one or more of the following therapies:
Treating underlying MDSIt usually involves supportive care, which aims to:
Supportive care is beneficial as most people with MDS are older adults who may have additional health problems.
Other possible treatments for MDS include occasional or more regular blood transfusions, which temporarily relieve anemia, fatigue, and bleeding. Blood transfusions work by increasing the number of red blood cells, platelets, or both in a person's blood.
MDS medications include ones that:
That said, stem cell transplants can provide a possible cure for some people. This involves replacing a person's damaged stem cells with healthy stem cells from a closely matched donor. A person with MDS may receive chemotherapy alongside a stem cell transplant or by itself.
Those waiting for a stem cell transplant or those ineligible for one may benefit from immunosuppressive therapy. This works on the immune system, slowing or stopping bone marrow damage.
Learn more about treating MDS.
A 2021 study states that despite many people seeing initial benefits from erythropoiesis-stimulating agents, many develop resistance to these medications over time and need blood transfusions.
Blood transfusions can help treat the anemia, but there can be downsides, such as iron buildup in the body. A person may then need iron chelation therapy. They can also experience higher healthcare costs and lower quality of life.
Doctors commonly use the Revised International Prognostic Scoring System (IPSS-R) to determine the outlook for someone with MDS. It takes into account the following:
Doctors can then assign a person to a risk group to estimate how likely they are to develop acute myeloid leukemia — a rare cancer of the bone marrow and blood — and their overall chances of survival.
The table below outlines overall survival times for MDS, as reported by the American Cancer Society:
MDS is a group of rare blood cancers that result in the bone marrow struggling to produce healthy blood cells, including red blood cells. In some people, MDS can lead to anemia.
Having anemia with MDS can lead to symptoms of fatigue, unusually pale skin, shortness of breath during activity, and dizziness, among others. Doctors may diagnose the condition based on results from blood tests, which show low levels of healthy red cells and other blood components.
Treatment focuses on treating symptoms and can include a combination of blood transfusions, stem cell transplants, immunosuppressive therapy, and medications.
A person's outlook depends on many factors, including how they respond to treatment and how advanced the MDS is.



Comments
Post a Comment