Silent Spring—III
Ashkenazi Jewish Genetic Disease Carrier Screening
Cite this articleGross, S., Pletcher, B., Monaghan, K. Et al. Ashkenazi Jewish genetic disease carrier screening. Genet Med 10, 461–462 (2008). Https://doi.Org/10.1097/GIM.0b013e31817102e1
Share this article Get shareable linkGenetic Testing Offers Options, Mom Says Ahead Of Tay-Sachs Awareness Month
Bonnie and Barry Davis were over the moon when they had their first child, Adam, a happy baby with an easy smile.
"We thought we had a perfectly healthy newborn, and everything seemed fine," Bonnie, who lives in Portland, Ore., told JNS.
Within a few months, however, it became clear that Adam was not meeting milestones associated with children his age.
The family's pediatrician assured the couple that Adam was just moving at his own pace. But Bonnie was convinced that something was wrong. That feeling intensified as she searched for answers to why her son couldn't sit up and reach for the Cheerios she put out for him.
Bonnie and Barry didn't know then that they were both carriers of the genetic disease Tay-Sachs, which is more prevalent among Ashkenazi Jews.
"A lot of Jewish people will hear about Tay-Sachs when they are growing up or in college, or their rabbis will advise couples to get tested, but we didn't," Bonnie said. "Even the American Gynecological & Obstetrical Society says that doctors are supposed to offer testing for Jewish couples, but we weren't."
Today, she serves on the board of the National Tay-Sachs and Allied Disease Foundation and spoke with JNS ahead of Tay-Sachs awareness month, which is held in September.
Still no cure, no treatment to slow progression
At 15 months old, Adam was diagnosed with Tay-Sachs, for which there is no cure. He died on Aug. 28, 2001, when he was just 2½ years old.
Adam Davis. Credit: Courtesy.One in 30 Jews of Ashkenazi and Eastern European descent is a Tay-Sachs carrier, and when both parents are carriers, the child has a 25% chance of developing the disease and a 50% chance of being a carrier. That's according to Karen Grinzaid, executive director of JScreen, a genetic testing and counseling nonprofit based at Emory University in Atlanta.
Fewer than 5,000 Americans have Tay-Sachs, according to an estimate by the National Institutes of Health.
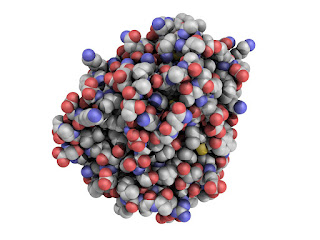
"People with Tay-Sachs disease do not have enough of an enzyme called beta-hexosaminidase A. The less enzyme a person has, the more severe the disease and the earlier that symptoms appear," per the NIH.
Tay-Sachs symptoms can appear at any point in life, but the most common severe form appears in the first few months of a baby's life. The symptoms include loss of learning skills, seizures, and muscle and mental function loss, as well as behavior problems and common respiratory infections, according to the NIH.
"There is no cure for Tay-Sachs disease, and no treatments are currently proved to slow progression of the disease," per the Mayo Clinic. "Some treatments can help in managing symptoms and preventing complications. The goal of treatment is support and comfort."
'Knowledge is power'
Tay-Sachs incidence has been particularly high on average among those of Eastern European and Ashkenazi Jewish descent, as well as among certain French Canadians, Pennsylvania Amish, Louisiana Cajuns and those of Irish ancestry, according to the Cleveland Clinic.
But those of any background can have Tay-Sachs, of which about one in 300 people is a carrier. Grinzaid, of JScreen, told JNS that many babies with Tay-Sachs are born to interfaith couples or those with no known Jewish background.
The nonprofit, which was founded in 2013, raises awareness of the importance of genetic disease testing. JScreen tests people remotely for more than 200 diseases, including Canavan, cystic fibrosis and familial dysautonomia. The test, which formerly required a blood sample, can now be done with saliva.
"Carrier screening is important for everyone planning to have children," Grinzaid told JNS. "If a carrier is healthy, they will have no idea what diseases they are a carrier for."
Partners who both carry Tay-Sachs can choose in-vitro fertilization and test pre-implementation to see if either the sperm or egg is viable, or they might opt to use donor sperm or eggs, according to Grinzaid. Some also decide not to have children, while others take their chances and test the baby in utero before deciding whether to continue the pregnancy, she added.
Testing used to require invasive blood work. Now, a saliva sample can be mailed to JScreen, where it is analyzed, after which genetic counselors hold telehealth meetings with parents to discuss the results and plan their options.
"Screening is knowledge," Bonnie Davis told JNS. "Knowing your carrier status is knowledge, and knowledge is power. You are entitled to have that knowledge."
The post Genetic testing offers options, mom says ahead of Tay-Sachs Awareness Month appeared first on JNS.Org.
Racist COVID Claims Spread By RFK, Jr., And Other Demagogues Are Deadly
Robert F. Kennedy, Jr., has floated a conspiracy theory that COVID "ethnically targeted" white and Black people and spared Ashkenazi Jewish and Chinese people. While this racist and antisemitic claim was, and is, easily debunked by global data on COVID cases and deaths, it was presented by Kennedy as a scientific theory and was widely circulated.
It's not the first time that claims about COVID have spread. Throughout the pandemic, similar claims have been made about genetic differences in susceptibility to COVID among populations. Each claim has proposed a unique biological reason why racial or ethnic groups have been more or less likely to be at risk of infection. As with Kennedy's nonsensical assertion about Jewish and Chinese people, these claims have been refuted by the data. COVID cases and deaths reveal that the likely drivers of differential susceptibility during the pandemic were poverty and having a job that made one more exposed to the COVID-causing virus.
Fear and bigotry make it surprisingly easy to convince people of racial and ethnic differences in disease susceptibility and reveal a deep, widespread misunderstanding about our shared vulnerability to illness. History has shown us time and again just how dangerous these ideas can be.
Kennedy's claims resonated precisely because they tapped into ideas about race and immunity that many people already carry around in their head. Even if people entertained Kennedy's assertions only for a moment—asking themselves, "Could it be true?"—they showed how powerful an idea the the presumption of a link between ancestry and immunity can be. After all, our immune system is based on our biology, which we inherit from our parents. Given this, it may seem a small leap to conclude there are shared features among racial or ethnic groups.
Unexamined, however, this line of thinking leads to the flawed idea that disease immunity, and any other biological characteristic, varies in clear and distinct patterns across racial and ethnic groups. As an epidemiologist and a historian, respectively, we think it important to talk about where those ideas come from—and why, in many cases, they bear little correlation to what either epidemiological science or medical history tells us about people's differential susceptibilities to infectious diseases.
First and foremost, susceptibility to such a disease is based on exposure. Without the pathogen (the disease-causing agent, whether it's a virus, a bacterium or some other microorganism), there is no risk. But as is the case with most infectious diseases, exposure to the pathogen alone is not sufficient to cause COVID: even when exposed to it, many people have mild symptoms or none at all. Because it was almost immediately recognized that the disease was caused by a coronavirus, and several viruses in this family were already circulating in human populations, questions soon arose about whether some populations might have prior immunity. What was, and remains, stunning is how little "evidence" it took for people to form opinions on which groups were protected or at risk.
As early as February 10, 2020, theories circulated online that East Asian individuals, particularly Chinese and Japanese people, were genetically susceptible to this coronavirus, called SARS-CoV-2. One article, written for the tourism industry, explained the evidence supporting this susceptibility came from a then preprint study of angiotensin-converting enzyme 2 (ACE2) receptors in only eight individuals, one of whom was Asian. Despite the weaknesses of such a small sample, the tourism industry article concluded with a susceptibility ranking for 30 unique racial and ethnic groups. At that time, very few cases of COVID had been reported outside of China. Italians from Tuscany were ranked by the author as among those with the lowest susceptibility. A month later Italy was in a lockdown, with hospitals overwhelmed.
The early claim that COVID was a disease unique to East Asians may have been driven by a combination of denial and fear—if only East Asians were susceptible, then no other racial or ethnic groups needed to worry. Many similar theories about racial immunity to COVID have circulated, each focusing on a different racial or ethnic group, particularly during the earliest days of the pandemic. It is likely that fear of the virus, and a desire to believe in the safety of oneself and one's family, helped fuel the spread of these claims. Conversely, the spread of these claims may have convinced people that precautions were unnecessary, thus further fueling the pandemic itself.
Obviously, it is a basic task of epidemiology to discern whether particular groups are more susceptible to a given disease or risk. That information forms the foundation for targeted interventions. Race, which is a social rather than biological categorization, and ethnicity are among the categories regularly used in such evaluations (along with age cohorts, occupation, geographical location, and so on). But framing disease susceptibility in those categories can backfire, giving people the impression that they are not among an at-risk group. Researchers at the University of Georgia found that, even in the absence of a biological explanation, knowing that Black communities and other communities of color experienced the highest death rates from COVID reduced empathy for those vulnerable to COVID and support for infection control measures among white Americans.
Theories about racial or ethnic differences in immunity or susceptibility to disease are not new. In the winter of 1347 the Black Death began its spread across Europe. By the spring of 1348, rumors were circulating that malefactors were deliberately causing the plague by poisoning wells. At the same time, violence started against Jewish people, including massacres of entire Jewish communities. By the late summer, well-poisoning accusations against Jewish communities spread faster than the disease; in some regions, violence erupted before a single case of the plague had occurred in the surrounding areas. Persecution and scapegoating were so widespread that in the summer of 1348 Pope Clement IV issued an official statement condemning the violence and stating that Jewish people were just as likely to die from the plague as Christians; the same message was reiterated in two additional statements from the pope that fall.
The lines we draw between racial and ethnic groups do not represent real biological differences in immunity. But fear and bigotry have revived this idea with every new pandemic. In a powerful speech at the Republican National Convention in 1992, Mary Fisher, a white, middle-class mother from Utah, reminded her audience that infectious disease knew no boundaries of class, race, or nationality. "HIV asks only one thing of those it attacks: Are you human?" she said.
COVID asks why we have yet to learn this lesson.
This is an opinion and analysis article, and the views expressed by the author or authors are not necessarily those of Scientific American.



Comments
Post a Comment