mRNA-based therapeutics: powerful and versatile tools to combat ...
Thrombocytopenia (Low Platelet Count)
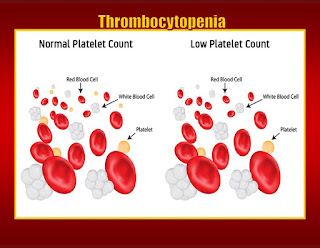
Thrombocytopenia is the condition when you don't have enough platelets in your blood. Platelets are small blood cells that clot your blood after you get any cut or scrape that bleeds or a bigger injury.These cells stick together, which stops bleeding.
You need platelets for your blood to clot. When your platelet counts are low, you may be at risk for bleeding.(Photo credit: Skypixel/Dreamstime)
If you're wondering what the long name means, here's how it breaks down: "Thrombocytes" is another name for your platelets, and "penia" means you don't have enough of something. Put those terms together, and you get "thrombocytopenia."
A healthy person usually has a platelet count of 150,000 to 450,000 in every microliter of blood. (A single drop of blood has about 35 microliters.) You have low platelets and thrombocytopenia if your lab values fall under 150,000.
Usually, you won't feel anything when you have thrombocytopenia. The condition often has no symptoms. But when you do have symptoms, they can include:
Thrombocytopenia has many possible causes. Sometimes it runs in families, but it's rare. Low platelet counts are more often related to one of many medical conditions or medicines you take for another condition. If your low platelet counts are caused by another condition, treating the underlying problem may help.
In general, anything that makes your body make less platelets than it needs will cause low platelet counts. You also can have low counts if your body is breaking platelets down or using them up faster than it's making new ones. Your platelet counts also can be low if your spleen or another part of your body is trapping platelets more than it should.
Conditions or things that can cause your body to make too few platelets include:
Conditions or things that can cause your body to break platelets down too fast include:
Conditions or things that can cause too many of your platelets to get lost or trapped include:
What are the most common low platelet count causes?
The most common reason for low platelet counts is another health condition or a medicine you're taking for another health condition. Some other risk factors for low platelets include:
You can have different types of thrombocytopenia depending on what's causing your low platelet counts:
Immune thrombocytopenic purpura (ITP)
One of the most common causes of low platelets is a condition called immune thrombocytopenia purpura (ITP). You may hear it called by its old name, idiopathic thrombocytopenic purpura. "Purpura" means that your skin looks purple like it's bruised. Although doctors don't know why ITP happens, the problem is that your immune system isn't working right. Your antibodies, which should attack infections, destroy your platelets by mistake.
ITP comes in two types: acute and chronic. Acute ITP usually happens in kids after a virus like chickenpox. It comes on fast and goes away in weeks or months. You probably won't need any treatment, and it usually won't come back. Chronic ITP means you'll have it for 6 months or more. Chronic ITP is more common in adults than it is in kids. But teens also can get it.
Thrombotic thrombocytopenic purpura (TTP)
TTP doesn't happen a lot, but it's dangerous when it does. When you have TTP, you'll get many blood clots throughout your body. These clots can make your organs not work right or damage them. The reason you'll have low platelet counts in your blood is that they're being used up in all the clots. TTP usually lasts for days, weeks, or even months. Without treatment, it can lead to brain damage, stroke, or death.
Drug-induced thrombocytopenia (DIT)
Medicines can cause low platelet count. This happens a lot, but doctors don't always realize a drug is why you have low platelet counts. More than 300 drugs can cause low platelets.
Usually you'll have this type of thrombocytopenia 1-2 weeks after you start a new drug. But certain drugs may cause it after you take it the first time. If a drug is causing your low platelet count, it usually will go away after you stop taking it.
Heparin-induced thrombocytopenia (HIT)
This type happens when you take a drug called heparin. Doctors use heparin to protect against blood clots when you're at risk for a dangerous clot due to surgery or another condition. It can happen when the drug makes your platelets clump up instead of staying in your blood. It usually happens 2-3 days after you take heparin the first time. Sometimes your immune system also plays a role. HIT is the most common type of DIT. It happens most often when you're in the hospital.
Gestational thrombocytopenia
This type is the most common cause of low platelets when you're pregnant. It's not clear why pregnancy causes low platelet counts. It happens most often late in pregnancy. It usually goes away after birth. But if you've had gestational thrombocytopenia with one pregnancy, it may come back if you get pregnant again.
Usually this type of thrombocytopenia doesn't lead to bleeding. But your doctor may want to order tests to make sure there isn't some other reason for your low platelet counts.
Dilutional thrombocytopenia
You can have low platelets after a major blood transfusion to replace more than all the blood you have in 24 hours. It happens when you've lost blood and platelets and then your blood is replaced with lots of red cells. If you have this, a doctor will decide if you need more platelets to get your count back up.
Distributional thrombocytopenia
This is the name for low platelet counts when your platelets get trapped in your spleen. Your spleen usually will have about 30% of your platelets in it. When your spleen is bigger than it should be, it can have up to 90% of your platelets.
Pseudothrombocytopenia
This type isn't thrombocytopenia at all. It happens when a problem with a blood test makes it look like your platelets are low when they really aren't. It usually isn't a problem, but it could be if you get more testing or treatment you don't need.
Thrombocytopenia is often found by chance when your doctor does a routine blood test. They might ask you questions to find out why your platelet counts are low and what type of thrombocytopenia you have.
Some questions your doctor may ask include:
Some tests check for low platelet counts or other things that may lead to low platelets:
Your doctor may do a physical exam to check you for signs of internal bleeding and feel if your spleen seems big. They may order an abdominal ultrasound to look for changes in your liver, spleen, or lymph nodes. You may also need genetic or other tests to help your doctor figure out why your platelets are low.
For most people, having a low platelet count isn't a big problem. But if you have a severe form, you can bleed even when you aren't hurt in your eyes, gums, or bladder. You also could bleed too much when you're hurt. You could bleed even with no injury at all.Trombocytopenia can be fatal, especially if you bleed a lot or bleed in your brain.
Thrombocytopenia Complications
If you have low platelets and don't follow your doctors advice, the condition can be life-threatening.
There are many treatment options for thrombocytopenia. If it's mild, you might not need any treatment. You'll need to work with your doctor to weigh the pros and cons of each and find a therapy that's right for you. The treatment will depend on what type of thrombocytopenia you have and what's causing it.
If your thrombocytopenia is drug-induced, stopping your medicine may help. If you have ITP and the trouble is with your immune system, your treatment depends on how severe a case you have. If it's mild, you may only need to get regular checks of your platelet levels.
When you do need treatment, the goal is to get your platelet count up enough to prevent serious bleeding in your gut or brain. You may need a platelet transfusion if there is immediate life-threatening bleeding. You may only get treatment when you have symptoms. But it's possible your doctor could suggest treatment even when you feel fine. That's more likely if you're at high risk for bleeding or other complications.
Some treatment options for low platelets include:
You can still do most things, but you may need to make some changes to your lifestyle to avoid getting hurt or cut. These include:
Your case may be different from someone else's. Your doctor will watch you to see how you're doing. If your thrombocytopenia is mild, you may not need any treatment. But even people who do need treatment can lead full lives.
Find out as much as you can about your condition and its causes so you can best manage it.
The Platelet Disorder Support Association has information about immune thrombocytopenia and other platelet disorders. They can help you connect to doctors, support groups, and other resources.
If you have thrombocytopenia, it means your platelets are lower than they should be. Low platelet counts can happen for many reasons, and your treatment will depend on what's causing your condition and how severe it is. Most people with thrombocytopenia won't have any symptoms or serious health risks. See your doctor or a blood disorder specialist (hematologist) to find out what's causing your low platelet counts and what steps you can take to protect your health.
Anything that leads you to have fewer platelets than you need can cause thrombocytopenia. Your immune system can cause it by attacking platelets. It's also caused a lot by medicines you're taking.
Most people with low platelet counts won't feel any different. But when your platelets are too low, you may bleed more than you should when you cut yourself. If you have a more severe case, ask your doctor what symptoms you should watch for.
Most people with low platelet counts will be OK even without treatment. Your thrombocytopenia may go away by itself, depending on what's causing it. Ask your doctor what tests you should get to see how severe your condition is, what's causing it, and whether treatment is needed.
What Is Thrombocytopenia?
Medically reviewed by Archana Sharma, DO
Thrombocytopenia is a platelet disorder that occurs when your blood platelet count drops too low. In adults, a normal platelet count typically ranges from 150,000 to 450,000 platelets per microliter of blood. However, if the count falls below 150,000, it is considered lower than normal.
Platelets, which are also called thrombocytes, are produced in the bone marrow from larger cells. When we get injured, these platelets team up and form a plug to seal the wound, called a blood clot or thrombus.
When your platelet count is low, it can become challenging to stop bleeding effectively. Bleeding can occur internally within the body, underneath the skin, or on the skin's surface. Serious bleeding complications usually arise when your platelet count becomes very low. Thrombocytopenia can potentially be life-threatening, especially if you have serious bleeding or are bleeding from the brain. It is crucial to seek early medical treatment to prevent serious complications.
Platelets can also activate when they sense a foreign invader in the body, releasing proteins to fight the infection. In addition to an increased likelihood of not being able to stop bleeding, thrombocytopenia may also lower your body's chances of successfully fighting the infection.
Researchers aren't exactly sure how many people have thrombocytopenia, as it is very likely underdiagnosed and underreported, and many people with it may be experiencing only mild symptoms.
Symptoms of ThrombocytopeniaThe main indicators of thrombocytopenia are associated with bleeding. You may not experience any symptoms, but if you do these symptoms can manifest suddenly or gradually develop over time. The condition is often discovered through a routine blood test.
Common signs of bleeding in thrombocytopenia may include:
Prolonged bleeding, even from minor injuries
Petechiae, which are small, flat red spots beneath your skin caused by leakage from your blood vessels
Purpura, or bleeding in the skin, resulting in red, purple, or brownish-yellow spots
Nosebleeds or bleeding from the gums
Blood in the urine (hematuria) or stool (hematochezia), causing it to appear as bright red or as a dark, tarry color
Heavy menstrual bleeding
Bruising
Thrombocytopenia is generally caused by one of three things. These are insufficient platelet production in your bone marrow, increased breakdown of platelets within your bloodstream, and increased breakdown of platelets in your spleen or liver.
Other conditions and factors can affect platelet production in you bone marrow, including:
Aplastic anemia, which occurs when your bone marrow fails to produce an adequate number of blood cells
Bone marrow cancers like leukemia
Cirrhosis, a condition characterized by liver scarring
Folate deficiency
Rare infections affecting the bone marrow
Myelodysplastic syndrome, which occurs when the bone marrow either makes too few healthy blood cells or produces defective cells
Vitamin B12 deficiency
Thrombocytopenia can also occur through the use of certain medications, including chemotherapy. A 2021 study reviewed data from over 15,000 patients and found that 13% of those being treated for solid tumors and 28% of those with haematologic malignancies, such as leukemia and Myelodysplastic syndrome, developed thrombocytopenia within the first three months of initiating chemotherapy.
Environmental exposure to toxic chemicals like pesticides, arsenic, and benzene can also impede healthy platelet production. Unhealthy lifestyle habits, such as excessive alcohol consumption, can temporarily lower your platelet count, especially in people with low vitamin B12 or folate levels.
DiagnosisTo diagnose thrombocytopenia, your healthcare provider will start by gathering information about your medical history and family background. They will also ask you about any symptoms you may be experiencing, and perform a physical examination to identify any signs of bleeding.
Your provider may think it's necessary to perform more blood tests. For example, a complete blood count, or CBC, may be ordered. This test measures the levels of platelets and other blood cells in your bloodstream. Another test your provider may order is a blood smear test. This involves placing a small sample of your blood on a slide and examining it under a microscope to further examine your platelets. Additionally, bone marrow tests may be ordered to assess the overall health of your bone marrow.
If your healthcare provider suspects that you have thrombocytopenia or another bleeding disorder, they may refer you to a hematologist. Hematologists specialize in diagnosing, treating, and managing blood-related conditions.
Treatments for ThrombocytopeniaThe treatment approach for thrombocytopenia varies depending on the underlying cause and the presence of symptoms. In cases of mild thrombocytopenia, treatment may not be necessary. However, if you are experiencing severe bleeding or have a high risk of complications, your healthcare provider may recommend various medications or procedures. Treating the underlying condition responsible for the low platelet count is also important, and will be part of the treatment regimen.
MedicationsSometimes medications can cause platelet levels to drop. If a reaction to a medication is the culprit behind your low platelet count, your provider may prescribe an alternate medication. For cases where your immune system is causing your low platelet count, your provider may prescribe medications that suppress your immune response (immunosuppressants).
Medications such as corticosteroids (e.G., prednisone) are commonly used to increase platelet count. Other medicines like Promacta (eltrombopag) and Nplate (romiplostim) can help stimulate platelet production. Monoclonal antibody medications such as Rituxan (rituximab) are medications that can aid in preventing your immune system from destroying platelets.
ProceduresIf medications are ineffective, certain procedures may be considered.
Blood or platelet transfusions are used for individual cases of heavy bleeding or among those at high risk of bleeding.
In some cases, surgical removal of the spleen, also called a splenectomy, may be recommended. The spleen stores platelets, and removing it can help improve your platelet levels in the bloodstream. However, this procedure carries potential risks, including bleeding, infection, and abnormal blood clots, so other treatment options may be offered first.
Reduce Your RiskWhile there aren't any ways to prevent thrombocytopenia, you can reduce your risk. Ask your healthcare provider about any medical conditions you have or prescribed medications you take that may increase your risk of thrombocytopenia. Work with them to create a treatment plan to reduce this risk, if possible.
Related ConditionsThrombocytopenia can be influenced by the following medical conditions:
Autoimmune disorders: These include immune thrombocytopenia (ITP), lupus, and rheumatoid arthritis, which can mistakenly trigger your immune system to attack and destroy platelets.
Cancer: This especially includes blood cancers such as leukemia or lymphoma. These types of cancers, and cancer treatments like radiation and chemotherapy, can damage your bone marrow and destroy blood stem cells.
Conditions that cause blood clots: These include thrombotic thrombocytopenic purpura (TTP) and disseminated intravascular coagulation (DIC).
Bacterial and viral infections: Thrombocytopenia can occur in chronic infections such as hepatitis B, hepatitis C, and human immunodeficiency virus (HIV).
An enlarged spleen: though rare, an enlarged spleen can be caused by certain conditions such as liver disease and leukemia.
Pregnancy: Mild thrombocytopenia can develop when you are close to delivery. It is possible to see a gradual decline in platelets from the first trimester until birth. This is attributed to the body's need to support the growing fetus.
Some surgical procedures: Platelets can be destroyed during surgical procedures involving artificial heart valves, blood vessel grafts, or the use of machines and tubing for blood transfusions or bypass surgery. This can occur as they pass through these artificial structures and equipment, leading to a decrease in platelet count.
The prognosis of thrombocytopenia varies and depends on the cause. The best way to prevent complications of thrombocytopenia is by working with your healthcare provider to establish a treatment regimen and determine what lifestyle changes you should make. Infection prevention measures should also be taken.
Tell your provider if you have any symptoms of an infection, such as a fever. Removing your spleen raises your risk of an infection. In this case, your provider may discuss taking steps to reduce your risk of infections, such as getting vaccinated. Monitor for symptoms of bleeding, which can quickly become a medical emergency.
If you are a smoker, then quitting smoking can make a huge difference in your health outcomes. Smoking can raise your risk of developing a blood clot.
Avoid contact sports, and ask your provider about physical activities that are safe for you. Take safety precautions, such as using a seatbelt while riding in a car and wearing gloves when working with knives and other tools.
Make sure to take all medicines as prescribed. Before any surgery or dental procedures, tell your healthcare provider about any medications you take that may lower your platelet count. These medicines may increase bleeding during these procedures. Avoid medicines that may lower your platelet count or stop your platelets from working properly. Aspirin and Advil (ibuprofen) are commonly used medicines that may thin your blood too much.
Frequently Asked QuestionsCan you live long with low platelets?
To manage low platelet levels and prevent complications, you should consult your healthcare provider. You may need routine testing to monitor your platelet levels and develop an appropriate treatment plan.
Is thrombocytopenia cancerous?
Thrombocytopenia itself is not cancerous, but it can be caused by cancers, like leukemia. It can also be caused by non-cancerous conditions, such as liver disease.
Is thrombocytopenia curable?
The treatment plan for thrombocytopenia varies based on the cause of this condition. If your platelet count is low because of a medication, for example, your healthcare provider may suggest switching to a different medication. Consult with your healthcare provider to identify what may be causing you to have thrombocytopenia.
For more Health.Com news, make sure to sign up for our newsletter!
Read the original article on Health.Com.
View comments
Aspirin 'safe' For Brain-bleed Strokes
By Michelle RobertsHealth editor, BBC News online
Patients who have had a stroke caused by bleeding in the brain can safely take aspirin to cut their risk of future strokes and heart problems, according to a new study.
Aspirin thins the blood and so doctors have been cautious about giving it, fearing it could make bleeds worse.
But The Lancet research suggests it does not increase the risk of new brain bleeds, and may even lower it.
Experts say the "strong indication" needs confirming with more research.
Only take daily aspirin if your doctor recommends it, they advise.
Aspirin benefits and risksAspirin is best known as a painkiller and is sometimes also taken to help bring down a fever.
But daily low-dose (75mg) aspirin is used to make the blood less sticky and can help to prevent heart attacks and stroke.
Most strokes are caused by clots in the blood vessels of the brain but some are caused by bleeds.
Because aspirin thins the blood, it can sometimes make the patient bleed more easily.
And aspirin isn't safe for everyone.
It can also cause indigestion and, more rarely, lead to stomach ulcers.
Never give aspirin to children under the age of 16 (unless their doctor prescribes it).
It can make children more likely to develop a very rare but serious illness called Reye's syndrome (which can cause liver and brain damage).
The studyThe research involved 537 people from across the UK who had had a brain bleed while taking anti-platelet medicines, to stop blood clotting, including aspirin, dipyridamole or another drug called clopidogrel.
The work is being presented at the European Stroke Organisation Conference in Milan.
What do experts say?The research cannot prove that aspirin prevents future strokes but it appears to be linked to a lower risk.
Nor does it suggest that aspirin is always safe to take.
But it hints that more patients - those with haemorrhagic or brain bleed strokes - might benefit from daily treatment.
It's not clear if the study findings will apply to all patients in real life.
Lead researcher, Prof Rutsam Salman, from the University of Edinburgh, said: "At the moment, people do not know what the right thing to do is.
"Doctors are hesitant about giving aspirin or aspirin-like drugs to people who have had this type of stroke.
"UK and European guidelines do not give any recommendation, because there hasn't been enough evidence.
"I think we have now confirmed safety with these findings.
"It certainly seems that aspirin is safe enough to give."
Prof Salman recommended more work to see if aspirin might actually lower the risk of brain bleeds as well as clots.
Prof Metin Avkiran, from the British Heart Foundation, which funded the research, said: "Around a third of people who suffer a brain haemorrhage, also known as haemorrhagic stroke, do so when they are taking an anti-platelet medicine, such as aspirin, to reduce the risk of a heart attack or an ischaemic [blood clot] stroke.
"We now have a strong indication they can carry on taking these potentially life-saving medicines after the brain haemorrhage without increasing the risk of another one, which is crucial new information for both patients and doctors."
Anyone with concerns should speak to a doctor before considering changing medication, however.
Preventing a strokeYou can reduce your risk by:
Copyright 2023 BBC. All rights reserved. The BBC is not responsible for the content of external sites. Read about our approach to external linking.
Beta Terms By using the Beta Site, you agree that such use is at your own risk and you know that the Beta Site may include known or unknown bugs or errors, that we have no obligation to make this Beta Site available with or without charge for any period of time, nor to make it available at all, and that nothing in these Beta Terms or your use of the Beta Site creates any employment relationship between you and us. The Beta Site is provided on an "as is" and "as available" basis and we make no warranty to you of any kind, express or implied.
In case of conflict between these Beta Terms and the BBC Terms of Use these Beta Terms shall prevail.



Comments
Post a Comment