*'Almost-perfect baby' era is coming*
'Genetic, Acquired Factors Can Cause Abnormal Blood Clotting'
Express News Service
Blood clotting disorders are conditions that cause blood to form clots too easily, potentially restricting the normal flow of blood within your body. Dr Deepak Charles, a consultant haematologist-oncologist, explains clotting disorders, prevention, and treatment methods.
Why does abnormal clotting occur?
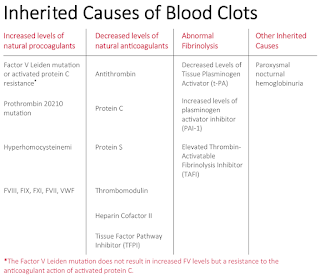
There are two types of clotting disorders commonly encountered. The most frequently observed is deep vein thrombosis (DVT), which occurs in the lower limbs. In this type, blood clots develop in one of the body's deep veins. The second type is pulmonary embolism, wherein a blood clot blocks an artery in the lung, halting blood flow. Both genetic and acquired factors contribute to abnormal blood clotting. Genetic factors encompass gene mutations and variations in protein levels. Acquired factors involve the presence of other diseases and the side effects of drugs and medications. Additionally, certain blood-related cancers can trigger abnormal clotting.
What are the trends post Covid-19?
During the pandemic, there was an increase in cases of clotting disorders. One cause was Covid-19 infection itself, as the disorder was observed in those affected by the virus. Furthermore, a connection was identified between clotting disorders and vaccines, particularly the two types available in India. However, after the pandemic, there has been a trend of decreasing case numbers.
Can it be identified early; if so, what are the preventive measures?
Early detection of the disorder is feasible through diligent monitoring. If the disorder is hereditary or if a family member has it, the likelihood of developing the disease is higher. Being attentive to changes and symptoms can aid in preventing its occurrence. Symptoms like swelling and unexplained pain should prompt consultation with a doctor for timely detection. It's important to note that clotting can occur anywhere in the body, not solely in the legs.
What are the treatment options?
The primary treatment for clotting disorders involves anti-clotting measures, which typically employ blood thinners. These medications can be administered orally or via injection. Additionally, minimally-invasive procedures can remove blood clots. This intervention employs specialized devices to effectively remove clots.
Blood clotting disorders are conditions that cause blood to form clots too easily, potentially restricting the normal flow of blood within your body. Dr Deepak Charles, a consultant haematologist-oncologist, explains clotting disorders, prevention, and treatment methods. Why does abnormal clotting occur? There are two types of clotting disorders commonly encountered. The most frequently observed is deep vein thrombosis (DVT), which occurs in the lower limbs. In this type, blood clots develop in one of the body's deep veins. The second type is pulmonary embolism, wherein a blood clot blocks an artery in the lung, halting blood flow. Both genetic and acquired factors contribute to abnormal blood clotting. Genetic factors encompass gene mutations and variations in protein levels. Acquired factors involve the presence of other diseases and the side effects of drugs and medications. Additionally, certain blood-related cancers can trigger abnormal clotting.Googletag.Cmd.Push(function() {googletag.Display('div-gpt-ad-8052921-2'); }); What are the trends post Covid-19? During the pandemic, there was an increase in cases of clotting disorders. One cause was Covid-19 infection itself, as the disorder was observed in those affected by the virus. Furthermore, a connection was identified between clotting disorders and vaccines, particularly the two types available in India. However, after the pandemic, there has been a trend of decreasing case numbers. Can it be identified early; if so, what are the preventive measures? Early detection of the disorder is feasible through diligent monitoring. If the disorder is hereditary or if a family member has it, the likelihood of developing the disease is higher. Being attentive to changes and symptoms can aid in preventing its occurrence. Symptoms like swelling and unexplained pain should prompt consultation with a doctor for timely detection. It's important to note that clotting can occur anywhere in the body, not solely in the legs. What are the treatment options? The primary treatment for clotting disorders involves anti-clotting measures, which typically employ blood thinners. These medications can be administered orally or via injection. Additionally, minimally-invasive procedures can remove blood clots. This intervention employs specialized devices to effectively remove clots.How Hemophilia Is Inherited And Genetic Testing Options
Hemophilia is a blood clotting disorder that can be inherited. Caused by changes in the X chromosome, hemophilia is an autosomal recessive genetic disorder.
Hemophilia is a genetic disorder that affects the clotting factors in the blood. If you have hemophilia, your blood does not clot as it typically would. You may experience significant bleeding with surgery or trauma.
Here's how hemophilia is inherited, who is more likely to have the disorder, and what tests may help with diagnosis.
Learn more about hemophilia.
Hemophilia A, also called factor VIII deficiency, and hemophilia B, also called factor IX deficiency, are inherited on the X chromosome in an autosomal recessive pattern. This means that you must inherit one affected X chromosome to have the condition — in this case, hemophilia.
Generally, individuals have either two X chromosomes or one X and one Y chromosome. These chromosomes determine sex characteristics, such as if you produce eggs or sperm, have a penis or a vagina, and many other traits.
If you have a Y chromosome, you are more likely to inherit the disorder because there are no genes for clotting factors on the Y chromosome. This means that if your X chromosome carries the genes for hemophilia, you will have the condition.
If you have two X chromosomes, you may be hemophilia carriers. If you inherit one affected gene, you may be a carrier but may not have the disorder. You must inherit two affected X chromosomes to develop it, making hemophilia rarer in individuals with XX chromosomes.
There are three scenarios for how a person may inherit affected genes.
Parent with XX chromosomes carries an affected geneIf the parent with XX chromosomes is the carrier of the affected gene and the parent with XY chromosomes does not, their children with XY chromosomes have a 50% chance of inheriting the disorder. Their children with XX chromosomes, on the other hand, have a 50% chance of carrying the affected gene.
Parent with XY chromosomes has hemophiliaIf the XY parent has hemophilia and passes on the affected gene, each of their XY children has a 0% chance of inheriting the disorder. However, their children with XX chromosomes have a 100% chance of carrying the affected gene.
Both parents have affected genesIf both parents carry affected genes, each of their XY chromosome children has a 50% chance of inheriting the disorder. Their children with XX chromosomes have a 50% chance of inheriting one affected gene and becoming carriers. Additionally, children with XX chromosomes have a 50% chance of inheriting two copies of affected genes and having hemophilia.
Your doctor may suggest genetic testing if you or your partner have a family history of hemophilia. Before becoming pregnant, this can be done with a blood test. Your doctor will take a blood sample and send it to a laboratory to analyze the clotting factors.
During pregnancy, your levels of factor VIII will rise, making it difficult for a blood test to determine if you are carrying the affected gene. Levels of factor IX do not rise. However, other hemophilia tests can be done during pregnancy to find out if your child will have hemophilia.
They include:
Symptoms may appear soon after birth or within the first year of a child's life. An infant may have bleeding in the head after delivery, or an infant with a penis may experience bleeding after circumcision.
Additional symptoms over time:
Blood tests are the primary means of diagnosis if a person is experiencing symptoms of hemophilia.
Tests include:
Hemophilia is treated by replacing the blood clotting factor, a protein that is missing from the blood. Treatments include injecting clotting factor concentrates into a person's blood through their veins.
These treatments can be used episodically to help specific bleeding episodes or prophylactically to prevent future bleeding episodes.
Other treatment options:
People with hemophilia may need treatment throughout life to prevent bleeding episodes. They may also need additional monitoring as they age. Experts share that people with hemophilia are more likely to develop other health issues, like heart disease, joint disease, and kidney issues.
That said, life expectancy for people with hemophilia may be similar to that of the general population. In one recent study, people with mild to moderate hemophilia lived only one year less on average than people who did not have the condition.
How common is hemophilia?Hemophilia A is four times more common than hemophilia B. Recent data suggests that up to 33,000 people assigned male at birth in the United States have hemophilia. The disorder impacts around 1 in every 5,000 births of people assigned male.
Why do people with XY chromosomes not pass hemophilia onto their offspring with XY chromosomes?People with XY chromosomes do not inherit an X chromosome from their XY parent. Instead, they inherit the Y chromosome, which does not carry the disorder.
Is hemophilia always genetically inherited?No. About one-third of people with hemophilia have no genetic link to other family members.
Hemophilia is inherited on the X chromosome. Having this disorder or carrying it does not guarantee that your child will inherit the affected genes.
If you have a family history of this disorder, make an appointment with your doctor. You may be referred to a genetic counselor so you can better understand the potential risks.
These Genetic Tests Are Now Part Of Tricare's Covered Benefits
Defense health officials have added six preconception and prenatal genetic tests to military members' health care benefits.
The lab tests that are now a Tricare covered medical benefit include one test per condition, per lifetime, for these genetic disorders:
The tests are approved retroactively back to Dec. 27, 2021, when a law went into effect specifying they would become part of Tricare's basic coverage. So, beneficiaries who have paid out of pocket for one of these screenings since that date can apply for reimbursement by contacting their Tricare regional contractor. Beneficiaries can also request that Tricare reprocess a claim that had been denied for a test during that time. The new policy took effect July 19.
"Preconception and prenatal carrier screenings help identify people at risk for having children with genetic conditions that may have a high level of death or a shortened life expectancy," said LaChanda Black, a Tricare management and program analyst, in a statement accompanying the Defense Health Agency announcement. "Providing families access to these screenings can help them make decisions when planning their family."
These six tests were previously part of the Laboratory Developed Tests Demonstration Project, but have been moved to become part of the Tricare benefit.
The demonstration project includes many other tests, however, and has been extended for another five years, through July 18, 2028. The program gives Tricare beneficiaries access to certain tests that aren't yet approved by the Food and Drug Administration.
According to a July 13 notice in the Federal Register, Defense Health Agency officials cite "an ever-expanding pool of non-FDA-approved LDTs, including tests for cancer risk, diagnosis and treatment; blood and clotting disorders; a variety of genetic diseases and syndromes; and neurological conditions."
Officials note that in some instances, "LDTs are important and necessary tests and, in many instances, there are no FDA-approved/cleared alternatives."
The agency started the demonstration project in 2014 to review non-FDA-approved laboratory developed tests to determine if they meet Tricare's requirements for safety and effectiveness, and otherwise meet Tricar's criteria for coverage. During the demonstration, DHA allows tests that meet such criteria to be covered as a benefit.
The project has been extended several times.
The non-FDA-approved tests covered under the demonstration are available under cost-sharing for eligible Tricare beneficiaries, but they must be performed by a laboratory that is assessed and certified or accredited under minimum quality standards set by the Centers for Medicare and Medicaid Services.
Beneficiaries should check with their provider or regional contractor to find out what tests are included in the demonstration.
The cost to extend the demonstration project for another five years is expected to total about $199 million, according to the Federal Register notice.
Karen has covered military families, quality of life and consumer issues for Military Times for more than 30 years, and is co-author of a chapter on media coverage of military families in the book "A Battle Plan for Supporting Military Families." She previously worked for newspapers in Guam, Norfolk, Jacksonville, Fla., and Athens, Ga.
Share:



Comments
Post a Comment