COVID-19 pandemic (2019-21)
Abnormal Uterine Bleeding May Be Caused By Clotting Factor Deficiencies
A new review article illuminates why physicians should keep coagulation disorders in mind when evaluating patients with heavy abnormal uterine bleeding.
Physicians treating patients with heavy menstrual bleeding (HMB) should consider the possibility that rare bleeding disorders and hemophilia carrier states are at play if other, more common causes of bleeding have been excluded, according to a new report.
The report, a literature review published in Life (Basel),1 outlines several coagulation disorders and offers physicians guidelines on how to spot and treat hemostatic disorders.
Authors explain that current literature suggests 10% to 35% of women experience HMB at some point during their reproductive years. There are several potential causes of such bleeding, and physicians can use the PALM-COEIN system to help identify the underlying cause.
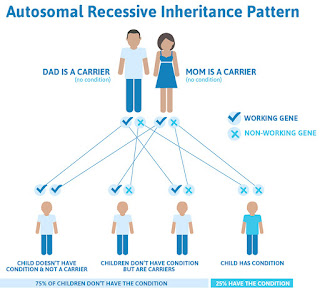
This system of abnormal uterine bleeding classification, from the International Federation of Gynaecology and Obstetrics,2 includes structural causes like polyps, adenomyosis, leiomyoma, malignancy, and hyperplasia, and functional causes, including coagulopathy, ovulatory disorder, endometrial disorders, iatrogenic conditions, or not-yet-classified causes. The existing literature suggests that an underlying inherited bleeding disorder is at play for 10% to 62% of adolescents with HMB. The most common such disorder is von Willebrand disease, but the authors said several other, less-common conditions should also be considered. Those less-common conditions are the focus of the review article.
The authors first reviewed several rare coagulation factor disorders. For instance, they said factor I, or fibrinogen, is a soluble plasma glycoprotein that in some patients is absent (congenital afibrinogenemia) or reduced (hypofibrinogenemia). In the former, patients can have a wide range of clinical manifestations, from minimal bleeding to serious hemorrhages, the authors said. Such patients may also experience arterial or venous thrombosis. In coagulation tests, partial thromboplastin time (PTT), prothrombin time (PT), thrombin time (TT) are all "infinitely prolonged," the authors said, since all of the parameters require the formation of fibrin.
Patients with hypofibrinogenemia are often asymptomatic if their fibrinogen levels are above 1 g/L, but the authors said these patients sometimes experience bleeding or thrombotic complications.
"In affected individuals, PT, PTT, and TT are variably prolonged, with TT being the most sensitive assay," they said.
Factor VII deficiency is believed to make up about one-third of rare coagulation disorders. The factor is vitamin K dependent and, like factor I, is synthesized in the liver and secreted in the plasma, the authors said. Patients with a deficiency of factor VII can have a wide range of manifestations, the authors said, "from asymptomatic or mildly symptomatic cases—for example, easy bruising, gum bleeding, and epistaxis—to severe cerebral and gastrointestinal hemorrhage."
Unfortunately, there are no clear treatment guidelines for factor VII deficiency, the authors said, although the published literature suggests a number of potential treatments, including surgery and blood transfusions.
Factor XIII deficiency is one of the rarest coagulation disorders, with only 500 cases reported globally since 1960, the authors said.
"Factor XIII is a transglutaminase that cross-links fibrin fibers between amino acid residues, hence stabilizing a fibrin clot," they wrote.
Patients with the deficiency can present with abnormal uterine bleeding, umbilical bleeding, or severe ovulation bleeding, among other clinical manifestations. However, the authors said factor XIII deficiency can be difficult to diagnose because clotting factor tests and platelet counts are normal in patients with the deficiency.
"The diagnosis can be made by measuring FXIII antigen levels using enzyme-linked immunosorbent assays and/or by measuring its activity with functional methods," the authors said. "Genetic testing of the genes encoding FXIII A or FXIII B is also an option for more specific assessment."
The authors also described several other disorders, including deficiencies of factors V, VIII, X, and XI, and hemophilia.
The investigators said they hope their report serves as a "useful guide" for physicians investigating abnormal uterine bleeding.
"We hope that this review can serve as a roadmap for busy clinicians to familiarize themselves with coagulation factor disorders as a cause of heavy menstrual bleeding and guide them towards more targeted research," they said.
They added, however, that theirs was not a systematic review, and therefore it should not be considered an exhaustive guide to diagnostic decisions.
References
1. Livanou ME, Matsas A, Valsami S, Papadimitriou DT, Kontogiannis A, Christopoulos P. Clotting factor deficiencies as an underlying cause of abnormal uterine bleeding in women of reproductive age: a literature review. Life (Basel). Published online June 5, 2023. Doi:10.3390/life13061321
2. Munro MG, Critchley HOD, Broder MS, Fraser IS; FIGO Working Group on Menstrual Disorders. FIGO classification system (PALM-COEIN) for causes of abnormal uterine bleeding in nongravid women of reproductive age. Int J Gynaecol Obstet. 2011;113(1):3-13. Doi:10.1016/j.Ijgo.2010.11.011
Von Willebrand Disease Directory
Von Willebrand disease is a genetic bleeding disorder that results from lack of a certain protein in the blood. There are three types: type 1, the most common type, where you are missing some of the von Willebrand factor; type 2, in which the factor does not work correctly; and type 3, the most severe deficiency. Symptoms of von Willebrand disease are nosebleeds, gum bleeding, heavy periods, frequent bruising, and taking a long time for blood to clot. Follow the links below to find WebMD's comprehensive coverage about how von Willebrand disease is caused, how to treat it, and much more.
View All
Comments
Post a Comment