Conditions | Www.childrenshospital.org
Making Genetic Prediction Models More Inclusive
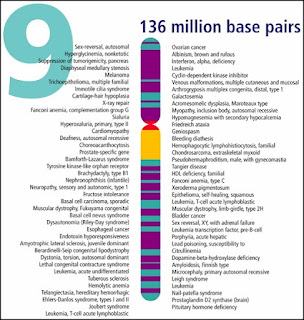
While any two human genomes are about 99.9% identical, genetic variation in the remaining 0.1% plays an important role in shaping human diversity, including a person's risk for developing certain diseases.
Measuring the cumulative effect of these small genetic differences can provide an estimate of an individual's genetic risk for a particular disease or their likelihood of having a particular trait. However, the majority of models used to generate these "polygenic scores" are based on studies done in people of European descent, and do not accurately gauge the risk for people of non-European ancestry or people whose genomes contain a mixture of chromosome regions inherited from previously isolated populations, also known as admixed ancestry.
In an effort to make these genetic scores more inclusive, MIT researchers have created a new model that takes into account genetic information from people from a wider diversity of genetic ancestries across the world. Using this model, they showed that they could increase the accuracy of genetics-based predictions for a variety of traits, especially for people from populations that have been traditionally underrepresented in genetic studies.
"For people of African ancestry, our model proved to be about 60% more accurate on average," says Manolis Kellis, a professor of computer science in MIT's Computer Science and Artificial Intelligence Laboratory (CSAIL) and a member of the Broad Institute of MIT and Harvard. "For people of admixed genetic backgrounds more broadly, who have been excluded from most previous models, the accuracy of our model increased by an average of about 18%."
The researchers hope their more inclusive modeling approach could help improve health outcomes for a wider range of people and promote health equity by spreading the benefits of genomic sequencing more widely across the globe.
"What we have done is created a method that allows you to be much more accurate for admixed and ancestry-diverse individuals, and ensure the results and the benefits of human genetics research are equally shared by everyone," says MIT postdoc Yosuke Tanigawa, the lead and co-corresponding author of the paper, which appears today in open-access form in the American Journal of Human Genetics. The researchers have made all of their data publicly available for the broader scientific community to use.
More inclusive modelsThe work builds on the Human Genome Project, which mapped all of the genes found in the human genome, and on subsequent large-scale, cohort-based studies of how genetic variants in the human genome are linked to disease risk and other differences between individuals.
These studies showed that the effect of any individual genetic variant on its own is typically very small. Together, these small effects add up and influence the risk of developing heart disease or diabetes, having a stroke, or being diagnosed with psychiatric disorders such as schizophrenia.
"We have hundreds of thousands of genetic variants that are associated with complex traits, each of which is individually playing a weak effect, but together they are beginning to be predictive for disease predispositions," Kellis says.
However, most of these genome-wide association studies included few people of non-European descent, so polygenic risk models based on them translate poorly to non-European populations. People from different geographic areas can have different patterns of genetic variation, shaped by stochastic drift, population history, and environmental factors—for example, in people of African descent, genetic variants that protect against malaria are more common than in other populations.
Those variants also affect other traits involving the immune system, such as counts of neutrophils, a type of immune cell. That variation would not be well-captured in a model based on genetic analysis of people of European ancestry alone.
"If you are an individual of African descent, of Latin American descent, of Asian descent, then you are currently being left out by the system," Kellis says. "This inequity in the utilization of genetic information for predicting risk of patients can cause unnecessary burden, unnecessary deaths, and unnecessary lack of prevention, and that's where our work comes in."
Some researchers have begun trying to address these disparities by creating distinct models for people of European descent, of African descent, or of Asian descent. These emerging approaches assign individuals to distinct genetic ancestry groups, aggregate the data to create an association summary, and make genetic prediction models. However, these approaches still don't represent people of admixed genetic backgrounds well.
"Our approach builds on the previous work without requiring researchers to assign individuals or local genomic segments of individuals to predefined distinct genetic ancestry groups," Tanigawa says. "Instead, we develop a single model for everybody by directly working on individuals across the continuum of their genetic ancestries."
In creating their new model, the MIT team used computational and statistical techniques that enabled them to study each individual's unique genetic profile instead of grouping individuals by population. This methodological advancement allowed the researchers to include people of admixed ancestry, who made up nearly 10% of the UK Biobank dataset used for this study and currently account for about one in seven newborns in the United States.
"Because we work at the individual level, there is no need for computing summary-level data for different populations," Kellis says. "Thus, we did not need to exclude individuals of admixed ancestry, increasing our power by including more individuals and representing contributions from all populations in our combined model."
Better predictionsTo create their new model, the researchers used genetic data from more than 280,000 people, which was collected by UK Biobank, a large-scale biomedical database and research resource containing de-identified genetic, lifestyle, and health information from half a million U.K. Participants.
Using another set of about 81,000 held-out individuals from the UK Biobank, the researchers evaluated their model across 60 traits, which included traits related to body size and shape, such as height and body mass index, as well as blood traits such as white blood cell count and red blood cell count, which also have a genetic basis.
The researchers found that compared to models trained only on European-ancestry individuals, their model's predictions are more accurate for all genetic ancestry groups. The most notable gain was for people of African ancestry, who showed 61% average improvements, even though they only made up about 1.5% of samples in UK Biobank. The researchers also saw improvements of 11% for people of South Asian descent and 5% for white British people. Predictions for people of admixed ancestry improved by about 18%.
"When you bring all the individuals together in the training set, everybody contributes to the training of the polygenic score modeling on equal footing," Tanigawa says. "Combined with increasingly more inclusive data collection efforts, our method can help leverage these efforts to improve predictive accuracy for all."
The MIT team hopes its approach can eventually be incorporated into tests of an individual's risk of a variety of diseases. Such tests could be combined with conventional risk factors and used to help doctors diagnose disease or to help people manage their risk for certain diseases before they develop.
"Our work highlights the power of diversity, equity, and inclusion efforts in the context of genomics research," Tanigawa says.
The researchers now hope to add even more data to their model, including data from the United States, and to apply it to additional traits that they didn't analyze in this study.
"This is just the start," Kellis says. "We can't wait to see more people join our effort to propel inclusive human genetics research."
More information: Yosuke Tanigawa et al, American Journal of Human Genetics (2023).
This story is republished courtesy of MIT News (web.Mit.Edu/newsoffice/), a popular site that covers news about MIT research, innovation and teaching.
Citation: Making genetic prediction models more inclusive (2023, October 26) retrieved 26 October 2023 from https://medicalxpress.Com/news/2023-10-genetic-inclusive.Html
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no part may be reproduced without the written permission. The content is provided for information purposes only.
A Mystery Disease Hit South Africa's Pine Trees 40 Years Ago: New DNA Technology Has Found The Killer
In the 1970s and 1980s, pine trees growing in various forestry plantations in South Africa's Western Cape province began to die in patches. These trees succumbed to a mysterious root disease and the patches expanded gradually. Spontaneous regrowth of seedlings in the patches died dramatically.
As in many other true crime dramas, the finger was initially pointed at the most likely suspect: the root-infecting Phytophthora cinnamomi. Its name – plant (phyto) destroyer (phthora) – reveals its power to cause harm; the pathogen is known to cause disease in almost 5,000 different plants.
After further investigation and the collection of many samples, tree pathologists shifted the blame onto the fungus Leptographium serpens (now known as Leptographium alacre). This fungus is well known to be transported by insects and was previously only known in Europe. It was visually identified from the roots of the dying trees. Now it was the prime suspect.
Doubts lingered, though. Most Leptographium species are not known to act as primary disease agents and so L. Serpens was most likely not able to cause the disease. Other fungi were also found within the roots of the diseased trees but could not be identified at the time due to a lack of more advanced techniques.
Knowing that the then-available technologies could not provide the complete answer to this mystery, the pathologists took more samples from the dead and dying pine trees, and stored them carefully. The hope was that one day they would have a better idea of the cause of this disease outbreak.
Fast forward to 2023 and a new character enters the mystery: DNA sequencing. This modern technology did what wasn't possible a few decades ago, allowing our team of molecular mycologists to identify the real culprit.
This tale is a testament to the ever-evolving nature of scientific inquiry. It reinforces the idea that, in the pursuit of knowledge, no stone should be left unturned and no assumption should be taken for granted. Through a blend of perseverance, technology, and a touch of serendipity, it was possible to solve a decades-old mystery.
Tracking a killerBack in the 1980s the samples were stored in the culture collection of the Forestry and Agricultural Biotechnology Institute at the University of Pretoria. In 2020, the samples were revived by a team that included ourselves and several others who recently published a paper on the topic.
We sequenced the samples' DNA to reveal their unique genetic code. By comparing this code against genetic databases, it was possible to figure out exactly what was causing the tree disease. And so, more than four decades after the disease was first described, the pathogen was finally identified as Rhizina undulata. L. Serpens, the long time primary suspect, was finally exonerated.
The culprit: Rhizina undulata Michael Wingfield, Author provided (no reuse)Rhizina undulata is well known to cause tree disease and death, mainly in Europe. This fungus is known colloquially as the "coffee fire fungus" because the intense heat caused by fires made by campers in a forest to brew coffee activates its dormant spores. This allows it to colonise the roots of conifers, including pines. R. Undulata is also well known in South Africa, where it kills many pines in the aftermath of forest fire and when trees are felled to clear a plantation.
What remains a mystery, however, is the trigger that activated this fungus in the Western Cape plantations. No fires were known to have occurred during the relevant time period.
One potential clue to the trigger may lie in the soil in which these trees were planted. Known as Table Mountain sandstone, this soil is sandy and acidic. Acidic soil has been shown in the laboratory to encourage R. Undulata growth. This naturally occurring acidity may have been the nudge the pathogen needed to infect the pine trees. It is also possible that the fungus was activated by heat radiating from the quartz rocks that are common in the areas in which the dying trees were planted.
It pays to be patientIn the years since the mysterious Western Cape outbreak, R. Undulata has become well known to foresters in pine plantations in other parts of South Africa and has done great damage to newly planted trees after fires. These fires can be accidental or due to what is known as slash-burning after trees are harvested.
Identifying R. Undulata as the culprit in those (no longer active) Western Cape plantations means scientists have more data that might help to better understand the biology of the fungus – which may lead to better control strategies in the future.
Our work is also a testament to the timeliness of scientific progress and the importance of patience. This story could only be fully unravelled when more advanced techniques were developed. It shows the power of modern technologies to solve historical problems. This underlines the need for continued investment into research and the development of new tools, both in South Africa and worldwide.
Our study also strongly advocates for the preservation of diverse fungal cultures for extended periods of time, regardless of their perceived importance at the time they are collected. The lack of accessible culture collections for lesser-known fungi, in South Africa and internationally, highlights the need for innovative approaches to safeguard these invaluable resources. This shift could revolutionise the study of microbes, opening new avenues beyond traditional species descriptions.
A Quick Genetic Test Offers Hope For Sick, Undiagnosed Kids. But Few Insurers Are Willing To Pay
Just 48 hours after her birth in a Seattle-area hospital in 2021, Layla Babayev was undergoing surgery for a bowel obstruction.
Two weeks later, she had another emergency surgery and then developed meningitis. Layla spent more than a month in neonatal intensive care in three hospitals as doctors searched for the cause of her illness.
Her parents enrolled her in a clinical trial to check for a genetic condition. Unlike genetic tests focused on a few disease-causing variants that can take months to produce results, the study at Seattle Children's Hospital would sequence Layla's entire genome, looking for a broad range of abnormalities — and potentially offer answers in under a week.
The test found Layla had a rare genetic disorder that caused gastrointestinal defects and compromised her immune system. The findings led doctors to isolate her, give her weekly infusions of antibiotics and contact other hospitals that had treated the same condition, said her father Dmitry Babayev.
Today, Babayev credits the test, known as rapid whole-genome sequencing, for saving his daughter's life. "It is why we believe Layla is still with us today," he said.
Like her disorder, Layla's experience is rare.
Few hospitalized babies with an undiagnosed illness undergo whole-genome sequencing — a diagnostic tool that allows scientists to quickly identify genetic disorders and guide clinicians' treatment decisions by analyzing a patient's complete DNA makeup. That's largely because many private and public health insurers won't cover the $4,000-to-$8,000 expense.
But an alliance of genetic testing companies, drugmakers, children's hospitals and doctors have lobbied states to increase coverage under Medicaid — and their efforts have begun to pay off.
Since 2021, eight state Medicaid programs have added rapid whole-genome sequencing to their coverage or will soon cover it, according to GeneDX, a provider of the test. That includes Florida, where the Republican-controlled legislature has resisted expanding Medicaid under the Affordable Care Act.
The test is also under consideration for coverage in Georgia, Massachusetts, New York and North Carolina, according to the nonprofit Rady Children's Institute for Genomic Medicine, another major provider of the test.
Medicaid coverage of the test can significantly expand access for infants; the state-federal program that insures low-income families covers more than 40 percent of children in their first year of life.
"This is an extraordinary, powerful test that can change the trajectory of these children's diseases and our own understanding," said Jill Maron, chief of pediatrics at Women & Infants Hospital in Providence, R.I., who has conducted research on the test.
"The only thing interfering with more widespread use is insurance payment," she said.
Proponents of whole-genome sequencing, which has been commercially available for about six years, say it can help sick infants with potentially rare diseases avoid a months- or years-long odyssey of tests and hospitalizations without a clear diagnosis — and increase survival.
They also point to studies showing rapid whole-genome testing may lower overall health costs by reducing unnecessary hospitalizations, testing and care.
But the test may have its limits. While it is better at identifying rare disorders than older genetic tests, whole-genome sequencing detects a mutation only about half of the time — whether because the test misses something or the patient does not have a genetic disorder at all.
And the test raises ethical questions because it can also reveal that babies — and their parents — have genes that put them at increased risk for adult-onset conditions such as breast and ovarian cancer.
Even so, some doctors say sequencing offers the best chance to make a diagnosis when more routine testing doesn't provide an answer. Pankaj Agrawal, chief of neonatology at the University of Miami Miller School of Medicine, said only about 10 percent of babies who could benefit from whole-genome sequencing are getting it.
"It is super frustrating to have sick babies and with no explanation what is causing their symptoms," he said.
Some private insurers now cover the test with certain limitations, including UnitedHealthcare and Cigna, but others do not.
Even in states that have adopted the test, coverage varies. Florida will add the benefit to Medicaid later this year for patients up to age 20 who are in hospital intensive care units.
Florida state Rep. Adam Anderson, a Republican whose 4-year-old son died in 2019 after being diagnosed with the rare genetic disorder Tay-Sachs disease, led the push for Medicaid to cover sequencing. The new state Medicaid benefit is named for his son, Andrew.
Anderson said persuading his GOP colleagues was challenging, given they typically oppose any increase in Medicaid spending.
"As soon as they heard the term 'Medicaid mandate,' they shut down," he said. "As a state, we are fiscally conservative, and our Medicaid program is already a huge program as it is, and we want to see Medicaid smaller."
Anderson said it took doctors more than a year to diagnose his son — an emotionally difficult time for the family as Andrew endured numerous tests and trips to specialists in several states.
"I know what it's like to not get those answers as doctors try to figure out what is wrong, and without genetic testing it's almost impossible," he said.
A Florida House analysis estimated that if 5 percent of babies in the state's neonatal intensive care units got the test each year, it would cost the Medicaid program about $3.3 million annually.
Florida's legislative leaders were persuaded in part by a 2020 study called Project Baby Manatee, in which Nicklaus Children's Hospital in Miami sequenced the genomes of 50 patients. As a result, 20 patients — about 40 percent — received a diagnosis, leading to changes in care for 19 of them.
The estimated savings exceeded $3.7 million — a nearly $2.9 million return on investment, after the cost of the tests, according to the final report.
"We have shown that we can justify this as a good investment," said Parul Jayakar, director of the hospital's Division of Clinical Genetics and Metabolism, who worked on the study.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF — the independent source for health policy research, polling, and journalism. This story also ran on CBS News. It can be republished for free.
If you purchase a product or register for an account through a link on our site, we may receive compensation. By using this site, you consent to our User Agreement and agree that your clicks, interactions, and personal information may be collected, recorded, and/or stored by us and social media and other third-party partners in accordance with our Privacy Policy.



Comments
Post a Comment